The Definitive Guide to Hashimoto's Thyroiditis: How Vitamin D, Selenium & Nutrition Can Revolutionize Your Treatment
Dive deep into the science behind Hashimoto's Thyroiditis. This expanded article, based on 5 scientific studies, breaks down the crucial role of Vitamin D, selenium, iodine & more. Discover dosages, mechanisms of action, and nutritional strategies to lower antibodies, improve thyroid function, and protect your cardiovascular health.
Nuri El azem De haro
10/19/20258 min read
Hashimoto's Thyroiditis: Redefining the Battlefield
Living with Hashimoto's Thyroiditis (HT) often feels like fighting a battle on two fronts. On one hand, there's managing the resulting hypothyroidism with levothyroxine, a vital hormone replacement strategy. On the other, there's the underlying cause: an autoimmune response where your own body attacks the thyroid gland. While levothyroxine is indispensable, it doesn't address the "why" behind this attack.
This is where modern science is opening an exciting new battlefront: immunonutrition. An overwhelming body of evidence, consolidated in the five studies we will analyze, demonstrates that what we eat and the micronutrients we supplement can directly modulate that immune response, calm inflammation, and potentially change the course of the disease.
This article is a deep dive into that evidence. We will break down, with detail and scientific rigor, how specific nutrients like vitamin D and selenium are not mere adjuncts, but central players on the complex board of thyroid autoimmunity.
The Universal Link: An Immune System Starved for Nutrients
All the analyzed studies start from a common, irrefutable premise: patients with Hashimoto's Thyroiditis show a significantly higher prevalence of deficiencies in key micronutrients, especially vitamin D and selenium, compared to the healthy population.
This correlation is much more than a simple coincidence. Vitamin D and selenium are potent immunomodulators, meaning they have the ability to direct and balance the activity of the immune system. A deficiency can leave the immune system dysregulated, promoting a chronic pro-inflammatory state that fuels the autoimmune fire against the thyroid. Therefore, correcting these deficiencies is not an option, but a fundamental piece of comprehensive treatment.
Deep Dive into Vitamin D: The Hormone Conducting the Immune Orchestra
Forget thinking of vitamin D just for bones. It actually functions as a sophisticated steroid hormone with receptors in almost every cell in the body, including—crucially—the cells of the immune system. Its role in modulating autoimmune diseases, especially HT, is so profound that it has become one of the most important areas of research.
The Mechanism of Action: How Does Vitamin D Calm the Immune System?
Vitamin D doesn't act simply; it's a master of cellular diplomacy. Its strategy is based on several pillars:
Rebalancing T-Cells: Imagine your immune system as an army. In HT, the pro-inflammatory "attack troops," known as Th1 and Th17 cells, are hyperactive. These cells secrete cytokines (chemical messengers) like Interferon-gamma (IFN-γ) and Interleukin-17 (IL-17), which orchestrate the assault on thyroid cells. At the same time, the "military police" of the immune system, the regulatory T cells (Treg), which should curb these attacks, are either fewer in number or less functional. Vitamin D intervenes directly to restore this balance: it inhibits the proliferation of Th1 and Th17 cells and, crucially, promotes the differentiation and function of Treg cells, restoring control to the system.
Suppressing Cytokines and Antigen Presentation: Vitamin D directly inhibits the production of pro-inflammatory cytokines by antigen-presenting cells (like dendritic cells). By doing this, it not only reduces inflammation but also decreases the ability of these cells to "present" thyroid antigens to T-cells, essentially reducing the "attack" signal.
The Genetic Factor (VDR Polymorphisms): Not everyone responds to vitamin D the same way. It has been discovered that certain genetic variations (polymorphisms) in the Vitamin D Receptor (VDR) gene, such as FokI, BsmI, and TaqI, are associated with a higher risk of developing Hashimoto's. This might mean that some individuals need higher serum levels of vitamin D to achieve the same immunomodulatory response, underscoring the need for a personalized approach.
The Evidence for Supplementation: Results from Meta-Analyses
Several meta-analyses have attempted to quantify the real impact of supplementation. The results, though mostly positive, present important nuances:
Antibody Reduction: The most robust and consistently demonstrated effect is a statistically significant reduction in anti-thyroid peroxidase antibodies (TPO-Ab). A meta-analysis of 12 randomized controlled trials (RCTs) confirms this strongly. Results for anti-thyroglobulin antibodies (TG-Ab) are also positive in broader analyses, although some individual studies didn't find as marked an effect. One large meta-analysis did find a significant reduction in both antibody types.
Improvement in Thyroid Function: Here the evidence is more heterogeneous. The meta-analysis by Tang et al. (2023) is very optimistic, showing that supplementation not only significantly decreases TSH but also increases levels of active hormones FT3 and FT4. However, the analysis by Jiang et al. (2022) found no statistically significant effect on these parameters. Why the discrepancy? It's likely due to differences in the duration of the included studies, dosages, the type of vitamin D used, and whether patients started with overt hypothyroidism or normal thyroid function.
Practical Supplementation Guide: Dose, Duration, and Type
Duration: Patience is a virtue. Studies are clear: treatment lasting longer than 12 weeks (>3 months) is significantly more effective in reducing TPO-Ab and improving FT4 and FT3 levels compared to shorter treatments.
Dose: There's no one-size-fits-all dose. Effective doses in studies range from 1200 to 4000 IU/day. The general recommendation is to supplement to reach and maintain blood levels (25(OH)D) within the optimal range for immune function, estimated between 40 and 80 ng/mL. This requires blood tests and professional adjustment.
Type of Vitamin D (Native vs. Active): This is a crucial distinction. Native vitamin D (cholecalciferol or D3) is commonly sold and needs activation by the liver and kidneys. The already active form is called Calcitriol. The meta-analysis by Tang et al. (2023) found that Calcitriol was significantly more potent in reducing TPO-Ab. However, Calcitriol is a medication that must be prescribed and monitored by a doctor, as it carries a higher risk of hypercalcemia. For general supplementation, Vitamin D3 is the preferred form.
Selenium: The Thyroid's Antioxidant Guardian
If vitamin D is the orchestra conductor, selenium is the thyroid gland's personal bodyguard. No other organ in the body has such a high concentration of this essential trace element.
The Mechanism of Action: How Does Selenium Protect the Thyroid?
Superior Antioxidant Defense: The process of creating thyroid hormones generates hydrogen peroxide, a molecule causing intense oxidative stress. Selenium is the central component of the enzyme glutathione peroxidase, the thyroid's most important antioxidant system. Without enough selenium, the thyroid damages itself every time it works.
Hormonal Activation: Selenium is vital for the deiodinase enzymes, which are responsible for converting T4 hormone (the storage form, mostly inactive) into T3 hormone (the active form used by cells). Selenium deficiency can lead to poor conversion and symptoms of hypothyroidism even with normal T4 levels.
Direct Immune Modulation: Like vitamin D, selenium has also been shown to modulate the balance of T-cells, helping to suppress the pro-inflammatory autoimmune response.
The Evidence for Supplementation: The Antibody Champion
The network meta-analysis by Peng et al. (2024), which directly compared the efficacy of various supplements, crowned selenium as the most effective.
Antibody Reduction: Selenium supplementation showed a very significant and consistent reduction in both TPO-Ab and Tg-Ab. This effect was robust and held across all sub-analyses, consolidating it as the most reliable nutritional intervention for this purpose.
Effective Dose: The most studied and consistently effective dose is 200 micrograms (µg) per day, preferably as selenomethionine due to its high bioavailability.
Intelligent Synergy: Myo-Inositol and Other Nutrients
Nutrition in Hashimoto's isn't just about isolated elements, but how they interact.
Myo-Inositol: The Signal Optimizer
Myo-inositol is a cyclic carbohydrate acting as a second messenger within cells, crucial for the thyroid cell to correctly "hear" the TSH signal.
Synergistic Effect: Studies show that Myo-inositol alone has a modest effect on antibodies. However, its true potential is unleashed in combination. Joint administration of Selenium and Myo-inositol has been shown not only to reduce antibodies but also to significantly decrease TSH levels in patients with subclinical hypothyroidism, helping many return to a euthyroid state (normal thyroid function). This combination is one of the most promising strategies for intervening in the early stages of the disease.
The Rest of the Essential Cast
Iodine: It's the thyroid's double-edged sword. Indispensable for hormone production , excess iodine (especially via uncontrolled supplements) can act as a catalyst that triggers or worsens the autoimmune response in susceptible individuals. The goal is to ensure sufficient (150 µg/day for adults) but not excessive intake, preferably from balanced dietary sources.
Iron: The thyroid peroxidase enzyme (TPO), which is attacked by TPO-Ab, is a "heme-enzyme," meaning it needs iron to function. Iron deficiency, extremely common in HT patients (often due to poor intestinal absorption), directly impairs thyroid hormone production and can cause anemia, worsening fatigue.
Zinc and Copper: These minerals are essential cofactors for hundreds of enzymatic reactions, including TSH synthesis, T4 to T3 conversion, and antioxidant protection. Zinc deficiency can reduce circulating T3 and T4 levels.
The Cardiovascular Connection: Protecting Your Heart
A crucial, often underestimated aspect of Hashimoto's Thyroiditis is its impact on cardiovascular health. The study by Mazur et al. (2025) delves into this connection.
Even subclinical hypothyroidism (elevated TSH with normal T4 and T3) already negatively impacts the heart. It is associated with altered lipid profiles (increased LDL cholesterol), increased systemic inflammation, arterial stiffness, and diastolic dysfunction (the heart's ability to relax and fill with blood). These factors significantly increase the long-term risk of developing cardiovascular diseases.
The nutritional interventions discussed, therefore, have a dual benefit: they not only help modulate thyroid autoimmunity but, by improving thyroid function and reducing inflammation, they also act as a preventive strategy to protect your cardiovascular health.
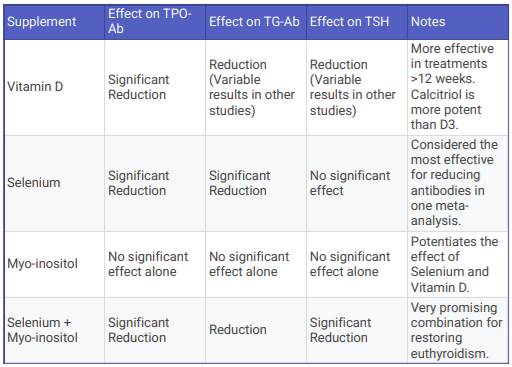
Summarizing table for a better overview
Figure 1. Effect of Vitamin D, Selenium, Myo-Inositol and Selenium + Myo-Inositol on TPO antibodies levels, TG antibodies levels and TSH levels.
The Action Plan: Integrating Science into Your Daily Life
The scientific evidence is clear and compelling. A modern, comprehensive approach to Hashimoto's Thyroiditis must go beyond the levothyroxine pill. Nutrition and targeted supplementation are powerful tools to modulate the immune response, reduce inflammation, and consequently, lower autoantibody levels.
Based on current evidence, an optimal approach could include:
Nutritional Audit and Lab Work: The first step is knowing your baseline. Ask your doctor for lab tests including: 25(OH)Vitamin D, Selenium in plasma or whole blood, and a complete iron profile with ferritin.
Evidence-Based Supplementation (under medical supervision):
Vitamin D: Supplement with Vitamin D3 to bring your levels into the optimal range (40-80 ng/mL). Doses of 2000-4000 IU/day are a good starting point. Be consistent: effects require at least 3-6 months.
Selenium: Consider daily supplementation with 200 µg of selenomethionine, the most proven strategy for reducing TPO-Ab and TG-Ab.
Strategic Combination: If you have subclinical hypothyroidism, discuss with your doctor the possibility of combining Selenium with Myo-Inositol (inositol dose in studies is often 600 mg).
Iron and Zinc: Correct any iron deficiency (ideally aiming for ferritin > 70 ng/mL) and ensure adequate zinc intake.
Adopt an Anti-Inflammatory Diet: Prioritize a dietary pattern like the Mediterranean Diet. This means: plenty of colorful and leafy green vegetables, fruits, legumes, fatty fish rich in omega-3s (salmon, sardines), extra virgin olive oil, nuts, and seeds. Minimize pro-inflammatory foods like ultra-processed items, refined sugars, and poor-quality fats.
Be Mindful of Iodine: Do not supplement with iodine unless you have a confirmed deficiency diagnosed by a professional. Obtain your iodine from balanced dietary sources.
The journey to managing Hashimoto's Thyroiditis is a marathon, not a sprint. Integrating these science-backed nutritional strategies, always in partnership with your medical team, empowers you not just to replace what's missing, but to calm the autoimmune storm at its source.
References
Peng, B., Wang, W., Gu, Q., Wang, P., Teng, W., & Shan, Z. (2024). Effects of different supplements on Hashimoto's thyroiditis: a systematic review and network meta-analysis. Frontiers in Endocrinology, 15, 1445878. doi: 10.3389/fendo.2024.1445878
Mazur, M., Szymańska, M., Malik, A., Szlasa, W., & Popiołek-Kalisz, J. (2025). Nutrition and Micronutrient Interactions in Autoimmune Thyroid Disorders: Implications for Cardiovascular Health. Pathophysiology, 32(3?). https://doi.org/10.3390/pathophysiology32030037
Tang, J., Shan, S., Li, F., & Yun, P. (2023). Effects of vitamin D supplementation on autoantibodies and thyroid function in patients with Hashimoto's thyroiditis: A systematic review and meta-analysis. Medicine, 102(52), e36759. doi: 10.1097/MD.0000000000036759
Soda, M., Priante, C., Pesce, C., De Maio, G., & Lombardo, M. (2024). The Impact of Vitamin D on Immune Function and Its Role in Hashimoto's Thyroiditis: A Narrative Review. Life, 14(6), 771. https://doi.org/10.3390/life14060771
Jiang, H., Chen, X., Qian, X., & Shao, S. (2022). Effects of vitamin D treatment on thyroid function and autoimmunity markers in patients with Hashimoto's thyroiditis-A meta-analysis of randomized controlled trials. Journal of Clinical Pharmacy and Therapeutics, 47(?), 767–775. doi: 10.1111/jcpt.13605